A brief introduction for newly-diagnosed patients
Diagnosis is confirmed by the presence of motor symptoms.
It denotes the beginning of the second stage of Parkinson’s.
Parkinson’s disease is diagnosed when the first motor symptoms appear. You may be told that this is the beginning of Parkinson’s disease. In fact, it is the beginning of the second stage of the disease. It represents a critical stage in disease progression when the loss of dopamine-producing neurons reaches a threshold (~70% loss), beyond which normal motor function is impaired. Most neurologists are only interested in the progression of these motor symptoms after diagnosis. However, disease progression is determined by the events that occurred during the so-called prodromal phase, which began up to 15 years before diagnosis and which continues to progress for the whole duration of the disease. These pre-diagnosis events cause non-motor symptoms, which are mistakenly considered side effects of Parkinson’s, when, in fact, they are the first signs of the root cause of the disease.
Neurologists use a model of Parkinson’s disease which focuses uniquely on motor symptoms. Non-motor symptoms are considered to be side effects – not really Parkinson’s at all.
The so-called prodromal phase of Parkinson’s disease precedes the appearance of motor symptoms by up to 15 years. This is the first stage of Parkinson’s. During this period, we can identify a number of conditions and processes occurring simultaneously:_
- non-motor symptoms originating in peripheral organs: first of all; constipation; later; nocturia and daytime urinary urgency,
- non-motor symptoms originating in the brain: fatigue, sleep disorders, brain fog, balance issues, apathy…
- the loss of ~70% of dopamine-producing neurons.
The common factor linking all these events is oxidative stress
Recent research has shown that all the non-motor symptoms listed above are attenuated when applying the Redox Stress Test developed by Dr. A. Wright, irrespective of their location. This indicates that these symptoms are the result of oxidative stress and mitochondrial dysfunction.
Cellular damage caused by oxidative stress.
The overall pattern of oxidative stress and mitochondrial dysfunction in several sites, including the brain, indicates that Parkinson’s is a syndrome best described as a multisystem redox disorder. In peripheral organs, this causes constipation and urinary urgency. In the brain, it causes fatigue, loss of balance, brain fog, and sleep impairment, as well as progressive neurological damage for the total duration of the disease.
Neurological damage caused by oxidative stress.
Early stage, pre-diagnosis. The symptoms generated by neurological damage are relatively mild, and the relationship between the symptoms caused by the cellular and neurological damage is not recognized.

Early stage Parkinson’s is defined uniquely by non-motor symptoms. Unfortunately, these are not recognized as symptoms of oxidative stress causing damage in neurons and peripheral organs.
Late stage, post-diagnosis. When left untreated for a long period, the accumulated neurological damage induces a dopamine deficiency that eventually exceeds the threshold required for normal motor control, creating a new coherent group of motor symptoms that define the condition as a movement disorder. Being only indirectly related to oxidative stress, these motor symptoms are indifferent to the Redox Stress Test. The neurological component of Parkinson’s Syndrome might therefore be considered a sequel to a relatively benign and treatable chronic multisystem redox disorder.
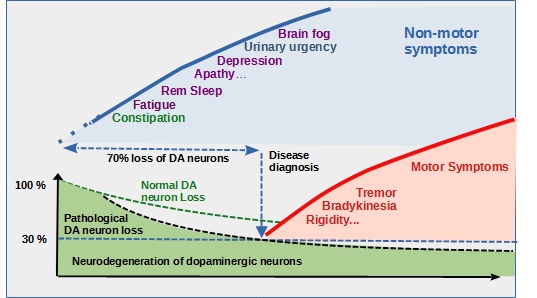
Late stage Parkinson’s begins when about 70% of dopaminergic neurons have been lost due to oxidative stress, and the first motor symptoms appear. This stage can be considered a sequel to early stage PD when left untreated.
Treatment Strategy
Early intervention to stop oxidative stress in all the sites where it is active is a prerequisite for controlling PD, starting with the gut and the lower urinary tract. This is a relatively easy task to achieve.
There is a reasonable chance that:
- If oxidative stress is stopped during the early stages, motor symptoms may never occur.
- If oxidative stress is stopped when motor symptoms are already present, further brain damage may be prevented.
Leave a comment