In this post I review the symptoms of Parkinson’s as defined by the “Idealized vision of Parkinson’s” promoted by the mainstream Parkinson’s Institutions and Charities and compare them to symptoms defined by my own observations, research and experimentation.
The Context
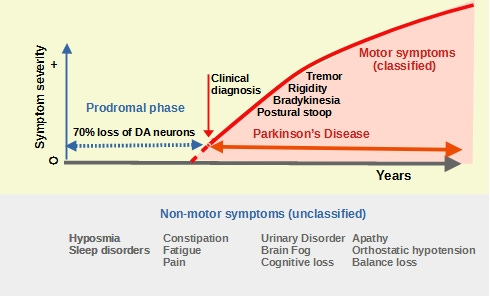
Parkinson’s Disease symptoms are currently divided into two groups of unequal value: Motor Symptoms are the cardinal signs which define Parkinson’s as a Movement Disorder and have their origin in areas of the brain that control movement. They are the basis of the clinical diagnosis of Parkinson’s by neurologists. “Motor symptoms are the signature of the movement disorder component of Parkinson’s disease.” All symptoms that cannot be identified as belonging to this group are dumped in the “unclassified bin” labeled “non-motor symptoms”. They originate in different organs, occur many years before motor symptoms and continue throughout the disease. As a result, they are ill-considered, misunderstood and often neglected. Only a minority of researchers and clinicians consider non-motor symptoms to be integral to Parkinson’s disease. As you will see, this non-classification profoundly hinders our efforts to understand the origin of Parkinson’s disease and its progression.
The “idealized vision” of Parkinson’s begins with the appearance of motor symptoms.
The period prior to diagnosis and any other symptoms are excluded from this interpretation.
Whereas for most health conditions, it is normal practice to explore the period before symptoms occur in an attempt to determine their origins and causes, this idealized vision of Parkinson’s firmly sets the chronological origin of the disease to coincide with the first appearance of motor symptoms and focuses attention on developments occurring thereafter. This restricted view of Parkinson’s is one of the reasons why the condition is misunderstood and its treatment has failed patients for so long.
Analysis
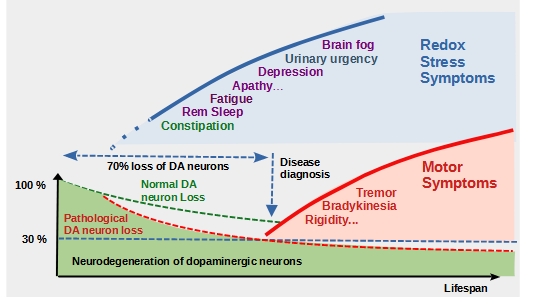
Taking a wider view of Parkinson’s, we see that many non-motor symptoms occur up to 20 years before clinical diagnosis. Sensory dysfunction with loss of sense of smell and pain is almost universal, as are disturbances of sleep-wake cycle. Autonomic dysfunction including orthostatic hypotension, urogenital dysfunction and constipation is also present to some degree in a majority of patients. From Poewe et al.
These symptoms are chronologically aligned with the loss of up to 70% of dopamine-producing neurons, which deprives the entire dorsal striatum, a brain region critical for motor program selection and coordination, of dopamine. At the time of first diagnosis, 30% or so of dopamine neurons and 50-60% of their axon terminals have been lost. There is therefore a substantial ‘window of opportunity’ to preserve what remains.
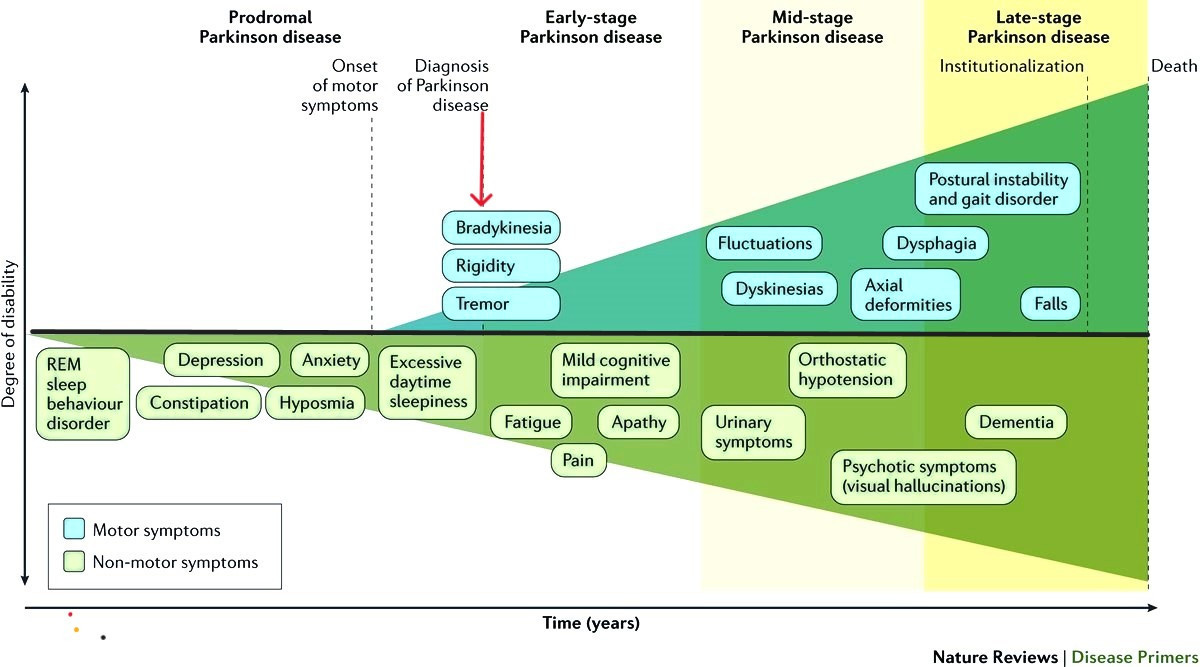
Non-motor symptoms appear many years before the clinical diagnosis of Parkinson’s. In this interpretation by Poewe et al., non-motor symptoms are fully integrated into Parkinson’s.
What causes the loss of dopamine-producing neurons?
DA neurons are particularly vulnerable to neurodegeneration because of their physical structure and size. Each dopaminergic neuron has a very extensive and complex axonal arborescence reaching from the substantia nigra (SN) to far into the striatum, delivering dopamine to more than a million synapses. The energy required to support this intense activity is provided by about 2 million mitochondria in the axons and synapses concerned. Any local mitochondrial dysfunction can lead to an energy shortage and degeneration of the more distant axons.
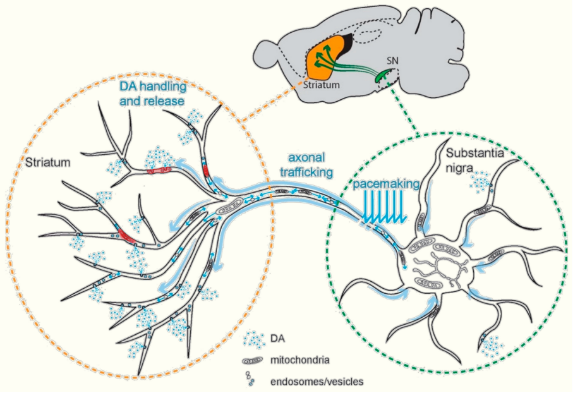
Schematic representation of a dopaminergic neuron showing axonal projections and factors contributing to its high bio-energetic demands. Image reproduced fromE Zampese and D J Surmeier.
Modest neuron loss occurs during healthy aging without severe neurological consequences because of the excess capacity of the DA network. Only rapid DA neurodegeneration caused by one or more exceptional events leads to the loss of more than 70% of the DA network that triggers motor symptoms.
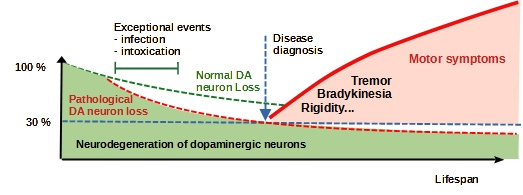
Normal (green dashed line) neuron loss with age does not lead to Parkinson’s. Excessive (red dashed line) DA neuron loss caused by exceptional events can lead to the loss of more than 70% of axons and the appearance of motor symptoms.
Whereas age contributes to slow non-pathological neuron loss, several conditions can contribute to more rapid, pathological neuron loss:
- intoxication due to pesticides (paraquat) or pollution (trichloroethylene),
- infection – Covid19, influenza…
- genetic mutations: LRRK2, PARK7, PINK1, PRKN, or SNCA,
- a modified profile of the gut microbiome which reduces the production of short-chain fatty acids such as butyrates and allows inflammation to increase in the intestines and the brain.
Two additional factors help complete the picture:
- All of these conditions lead to an increase in oxidative stress and mitochondrial dysfunction which in turn contributes to the loss of dopamine neurons through the action of aggressive free radicals and energy starvation.
- Non-motor symptoms of Parkinson’s are chronologically aligned to this exceptional loss of DA neurons.
Hypothesis
The association of these two factors suggests that non-motor symptoms might be markers of pathologies that drive the progression of Parkinson’s.
How can we test this hypothesis?
The Redox Stress Test is an analytical technique based on Broccoli Seed Tea, designed to establish whether symptoms are sensitive to changes in the oxidation state of their source. The Redox Stress Test activates the Master Regulator of Redox homeostasis, also known as the Nrf2 pathway in cells that are susceptible to oxidative stress. This neutralizes aggressive free radicals and restores normal levels of oxidation and mitochondrial health. In a pilot self-administered study, People with Parkinson’s prepared and ingested Standardized Broccoli Seed Tea once per week and monitored their symptoms over a six week period. They reported a rapid decline in non-motor symptoms whereas motor symptoms were strictly unaffected.
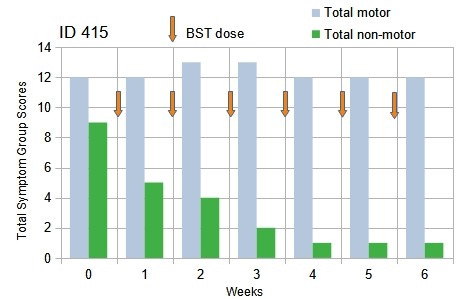
The Redox Stress Test: People with Parkinson’s reported a rapid decline of total non-motor symptoms whereas motor symptoms were strictly unchanged over the 6-week duration of the test.
The symptoms most strongly attenuated were: urinary urgency, constipation and fatigue, whereas brain fog/confusion, apathy and sleep impairment were partially attenuated.
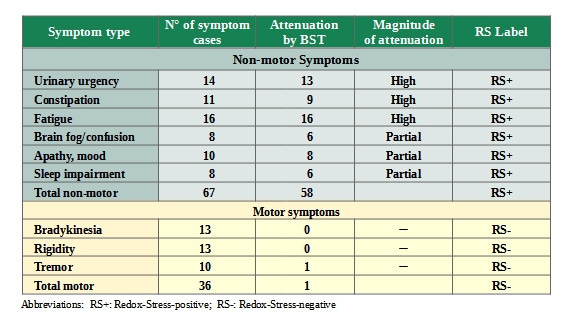
Self-assessed symptom response: Extracted from the records of 17 volunteers following self-administered consumption of freshly-brewed Broccoli Seed Tea for 6 weeks.
What does this tell us about these symptoms and about Parkinson’s disease?
- These previously unclassified symptoms are all sensitive to a reduction in oxidative stress in the cells of the organs concerned,
- They are the expression of cells suffering from a common pathology where aggressive chemical agents (collectively called reactive oxygen species, (ROS)) cause severe damage to membranes, DNA and mitochondria in the cells of the organs concerned.
- The pathology at the origin of these symptoms, as the Redox Stress Test demonstrates, can be halted in just a few weeks.
- No approved therapies exist to treat the underlying pathologies which cause these symptoms.
- These symptoms form a coherent group, which we can label Redox Stress Symptoms.
- They occur in 3 different biological systems:
- The Central Nervous System (CNS),
- The gastrointestinal (GI) tract
- The lower urinary tract (LUT).
- Given that they are present for the whole duration of the disease, Redox Stress Symptoms are the dominant symptoms of Parkinson’s disease.
- Redox Stress Symptoms are the markers of the pathologies that drive both the early stages and the progression of Parkinson’s disease.
- Overall, Parkinson’s corresponds to a multi-system redox disorder and would be better described as Parkinson’s Syndrome.
Chronologically, oxidative stress and mitochondrial dysfunction in multiple systems is the first pathology of Parkinson’s syndrome. The loss of DA neuron and subsequent dopamine depletion in the striatum are both sequels to that pathology in the brain which progressively destroys DA axons and neurons and ultimately wrecks the neuronal network.
Hierarchically, Redox Stress Symptoms are the parents of Motor Symptoms.
Functionally, Redox Stress Symptoms are the expression of the active pathology which drives disease progression. Motor Symptoms are the expression of the damaged state of the neuron network.
The failure of mainstream Parkinson’s Institutions and
Charities to recognize the importance of non-motor Symptoms
is a missed opportunity in the fight to develop
new therapies to treat Parkinson’s.
How does this reflect on the “idealized vision” of Parkinson’s currently promoted by mainstream Parkinson’s Institutions and charities?
The “idealized vision” defines Parkinson’s in terms of the damaged state of the neuron network and therapies to compensate for the effects of that damage but ignores the active pathologies that cause the damage.
It should come as no surprise to, learn that
focusing research on the state of the
network without addressing the pathologies
that are destroying it, is bound to fail.
This reclassification of Parkinson’s symptoms gives rise to a new model for Parkinson’s Syndrome
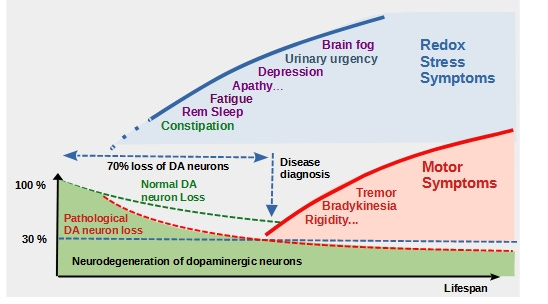
This new model helps clarify our understanding of Parkinson’s
Parkinson’s syndrome is defined by 2 pathologies
(i) Redox Disorder in peripheral organs and in the brain
(ii) Neurodegeneration in the brain and most likely in peripheral nervous systems.
- Multisystem Redox Disorder occurs over the entire duration of the disease and is responsible for Redox Stress symptoms.
- Neurodegeneration is a sequel to Redox Disorder in the brain and causes motor symptoms when about 70% of DA neurons are lost.
Nothing is quite as it seems in Parkinson’s
Leave a comment