… it is the simultaneous expression of two distinct pathologies.
In this post, I present arguments and evidence to demonstrate that describing Parkinson’s as a single disease is inaccurate and misleading. It is more accurate and much more helpful to describe Parkinson’s as two quite distinct pathologies which occur in a specific sequence, but then progress in parallel. The first to appear is a metabolic disorder resulting in oxidative stress at the cellular level of organs in different parts of the body including the brain. The second is a neurological disorder resulting from excessive neuron loss and damage to the neuronal network caused by the first pathology. The two pathologies then progress in parallel, the first driving the second.
This description becomes strikingly obvious once the nature, origin and chronology of all Parkinson’s symptoms are analysed in relation to disease progression. Unfortunately, understanding the nature and origin of many Parkinson’s symptoms has been hindered by the system used to classify them. Notably, classifying Parkinson’s symptoms into motor and non-motor symptoms, the latter by simple exclusion from the former, is particularly unhelpful. Reclassifying Parkinson’s symptoms according to their underlying pathologies is an essential step in building this description.
Parkinson’s symptoms
You are all familiar with the two groups of Parkinson’s symptoms. These are currently classified into two groups of unequal value, motor symptoms and non-motor symptoms. This classification is unsatisfactory and needs to be changed.
Motor Symptoms, the cardinal signs of Parkinson’s. Until now, only motor symptoms have been well classified and clearly linked to the neurological disorder created by the loss of a large part of the neuron network in the brain that generates and uses on the neurotransmitter, dopamine. Motor Symptoms are the cardinal signs which define Parkinson’s as a Movement Disorder. They have their origin in areas of the brain that control movement and are the basis of the clinical diagnosis of Parkinson’s by neurologists.The current description of Parkinson’s sets the chronological origin of Parkinson’s disease to coincide with the first appearance of motor symptoms and focuses attention on developments occurring in the brain thereafter. At this point the two pathologies are already very well established.
Non-Motor Symptoms, declassified, disregarded and misunderstood. All other Parkinson’s symptoms that are deemed not to belong to the motor symptom group are declassified and labelled “non-motor symptoms”. At first sight, these symptoms appear to be unrelated to each other since they are highly diverse in nature and originate in different bodily systems. Only a minority of researchers and clinicians consider non-motor symptoms to be integral to Parkinson’s disease. This lack of interest in such a large group of Parkinson’s symptoms profoundly hinders our efforts to understand the origin of Parkinson’s disease and its progression. Chronologically, many non-motor symptoms appear up to 20 years before the clinical diagnosis of Parkinson’s disease which is based uniquely on motor symptoms. Chronic fatigue, daytime sleepiness, pain, disturbances of the sleep-wake cycle, brain fog, loss of balance, constipation and loss of sense of smell are almost universal. Orthostatic hypotension, depression, and urinary disorders are frequent.
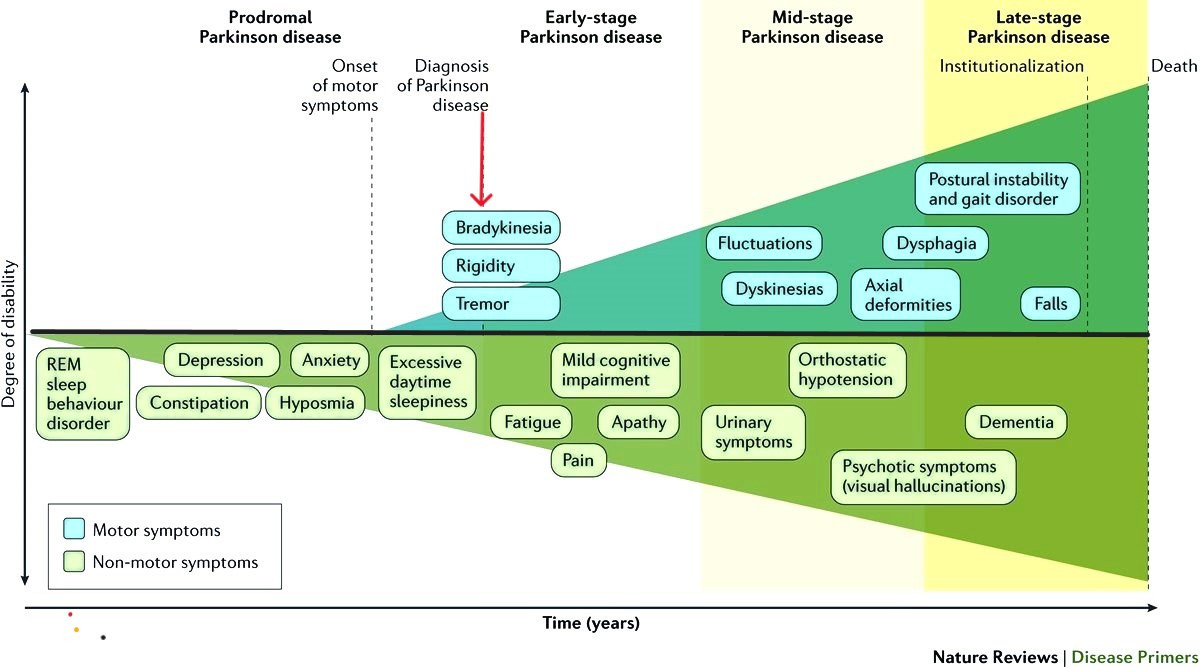
Several non-motor symptoms appear many years before the clinical diagnosis of Parkinson’s. In this representation by Poewe et al., non-motor symptoms are fully integrated into Parkinson’s disease.
The early non-motor symptoms, those which occur in the absence of motor symptoms, are chronologically associated with the loss of up to 70% of dopamine-producing neurons, which deprives the entire dorsal striatum, a brain region critical for motor function and coordination, of dopamine. At the time of first diagnosis, 30% or so of dopamine neurons and 50-60% of their axon terminals have been lost. These early non-motor symptoms are therefore the external signs of an underlying pathology that is quietly destroying a major neuronal network.
The Redox Stress Test
Non-motor symptoms are associated with a common pathology – oxidative stress. In a recent experiment, a group of People with Parkinson’s tested the effects of a herbal beverage designed to reduce oxidative stress in cells. The Redox Stress Test is an analytical technique based on a Broccoli Seed Tea containing a therapeutic dose of sulforaphane designed to activate the Nrf2 transcription factor, also known as the Master Regulator of Redox Homeostasis. By activating Nrf2, sulforaphane neutralizes aggressive oxidising agents and restores the normal levels of oxidation and mitochondrial health to the affected cells. The aim of the experiment was to establish whether attenuating oxidative stress might have an impact on symptoms of Parkinson’s disease. In a pilot self-administered study, People with Parkinson’s prepared and ingested Standardized Broccoli Seed Tea once per week and monitored their symptoms over a six week period. They reported a rapid decline in a wide range of non-motor symptoms whilst motor symptoms were unaffected.
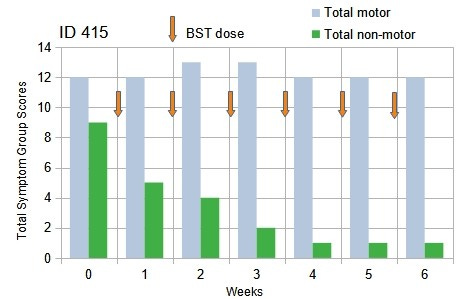
The Redox Stress Test: People with Parkinson’s reported a rapid decline of total non-motor symptoms whereas motor symptoms were strictly unchanged over the 6-week duration of the test.
The symptoms most strongly attenuated were: urinary urgency, constipation and fatigue, whereas brain fog/confusion, apathy and sleep impairment were partially attenuated. Most importantly, motor symptoms were strictly unaffected.
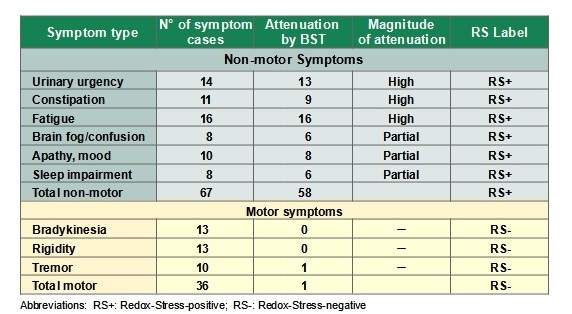
Self-assessed symptom response:Extracted from the records of 17 volunteers following self-administered consumption of freshly-brewed Broccoli Seed Tea for 6 weeks.
Although these results remain to be confirmed, we can tentatively reclassify the responsive non-motor symptoms as the expression of cells/organs suffering from oxidative stress and mitochondrial dysfunction. As such they form a coherent group of symptoms which should be renamed to reflect this condition. Using this classification, these two groups of Parkinson’s symptoms have different chronologies and are sensitive to different therapeutic treatments in a way which is mutually exclusive. Non-motor symptoms are sensitive to changes in the redox state of the cells concerned and insensitive to dopamine replacement therapy. Motor symptoms are sensitive to dopamine replacement therapy and insensitive to redox states. Taken together with the chronology of their occurrence, this clearly indicates that the two symptom groups are totally independent, and are the expression of two quite different different pathologies.
We can label these two pathologies of Parkinson’s as Primary and Secondary Parkinson’s disease to reflect the relation between the two pathologies.
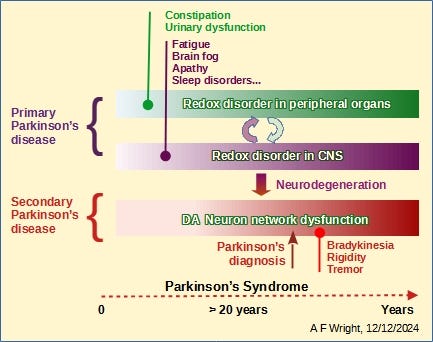
Timeline of the dual pathologies of Parkinson’s showing Redox Stress in peripheral organs spreading to the brain while expressing non-motor symptoms. The long-term effect of redox damage in neurons is the partial breakdown of the dopamine neuron network which triggers the occurrence of motor symptoms.
Two very different pathologies
The two pathologies are quite different in their nature, scale, symptoms and chronology.
The first pathology is oxidative stress, a metabolic disorder occurring at the cellular level. Oxidative stress occurs inside cells, affecting in particular the GI tract and the Lower Urinary tract and contaminating astrocytes and neurons in the brain. This disorder is chronologically associated with the occurrence of non-motor symptoms of Parkinson’s. It results from the formation of highly aggressive oxidizing chemicals (Reactive Oxygen Species, ROS) inside the mitochondria of cells in organs which have a high energy and oxygen consumption. These oxidants attack and damage the mitochondria which produce them as well as cell membranes and cellular DNA, ultimately leading to cell death. This is explained in more detail here.
The impact of this damage is fundamentally different when it occurs in neurons compared to when it occurs in cells of peripheral organs for a very simple reason: In peripheral organs damaged cells are rapidly replaced by new ones, whereas in the brain, neurons are not replaced or renewed.
In consequence, oxidative stress in the brain is a particularly serious problem, since it permanently damages the network of neurons affected by it.
The second pathology is neurological. Itis confined to the brain and is the direct result of the primary pathology. It develops on the scale of the network of neurons that produce the neurotransmitter dopamine, principally, but not exclusively, affecting parts of the brain that control movement. It is the result of the accumulated damage by ROS to the dopaminergic neuron network over decades. This pathology is therefore a sequel to the primary pathology and is expressed as motor symptoms of Parkinson’s.
The second pathology not only affects physical movement of the patients which limits their capacity to work, to exercise, to have a normal social life, even to eat, digest food and sleep normally, but also disrupts the messaging between the CNS and organs that control all other bodily functions. Overall, the combination of the two pathologies accelerates the progressive decline of the health, the quality of life and overall well-being of Parkinson’s patients.
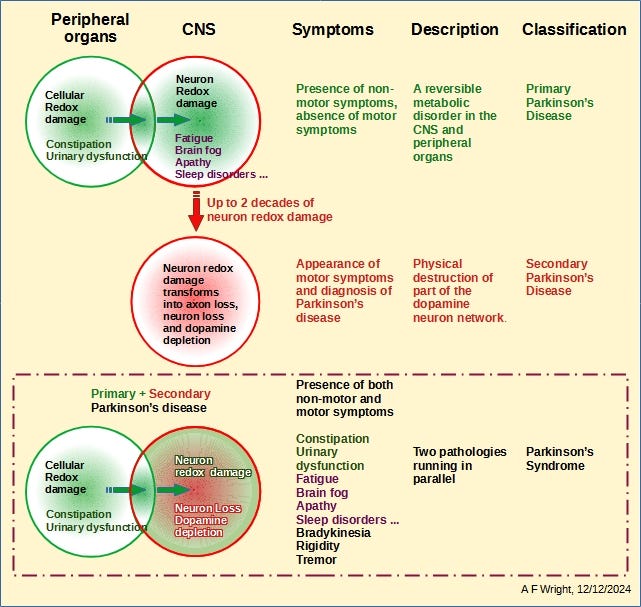
Primary Parkinson’s disease is the expression of oxidative stress in both peripheral organs and neurons. This is a metabolic disorder that can be resolved or reversed by activating the Nrf2 pathway to reset redox states in cells and neurons to normal levels.
Secondary Parkinson’s disease is the expression of a neurological dysfunction caused by the destruction of parts of the dopaminergic neuron network by the Primary Pathology of Parkinson’s disease over many years.
Parkinson’s disease, as experienced by most people post-diagnosis, is a combination of the two pathologies, expressing both motor and non-motor symptoms.
The Current State of care for Parkinson’s Disease
For the past 4 decades both care and research have been focused on neurological aspects of Parkinson’s disease. This approach has failed to deliver tangible benefits for patients.
The representation of Parkinson’s disease presented here leaves no doubt about the difficulty of resolving the neurological aspects of Parkinson’s disease without first resolving the metabolic aspects of the disease. It also indicates that focusing on the metabolic aspects could bring considerable relief to Parkinson’s patients by reducing the burden of non-motor symptoms.
What can we do about it?
It is time to rethink Parkinson’s and change the focus of both care and research to resolving Primary Parkinson’s disease.
Ignoring Primary Parkinson’s disease is accepting that disease progression cannot be slowed or stopped.
Primary Parkinson’s disease can be stopped/reversed.
Tell your Neurologist or Care provider that you are not satisfied with your current treatment and that more can be done.
Spread the word: “Parkinson’s is not a single disease …”
I am willing to work with any organisation, group or individual to help create the change needed to improve the wellbeing of Parkinson’s patients worldwide.
Dr Albert F Wright

Leave a comment